Australia’s alcohol and other drug treatment services can’t meet demand
Media Release
- Home
- News and Media
- Latest News and Announcements
- Australia’s alcohol and other drug treatment services can’t meet demand
April 2019
New data released today shows that more than 130,000 Australians received help from public alcohol and other drug treatment services in 2017-18, but up to another 500,000 people can’t get the help they need according to St Vincent’s Health Australia.
The data is contained in the Alcohol and other drug treatment services in Australia 2017–18 key findings, and shows alcohol is the most common drug people received treatment for, accounting for almost 69,000 of the 210,000 treatment episodes provided, more than one-third.
But alcohol and other drug experts say that while it’s good news Australians are putting their hands up for treatment, up to another 500,000 can’t get the help they need.
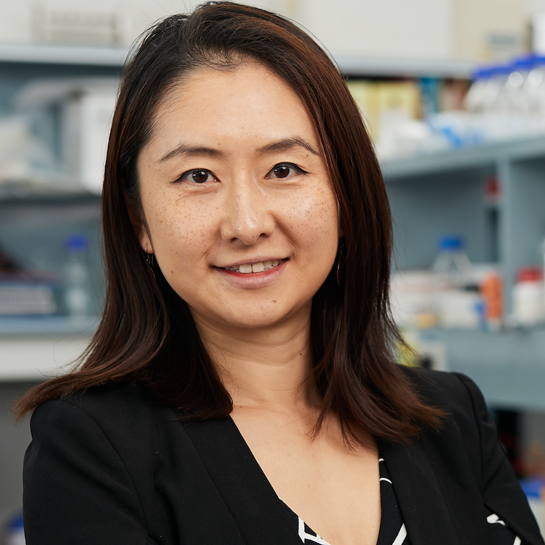
“Up to half a million Australians can’t access the alcohol and other drug treatment help they need – the services simply aren’t there or the waiting lists are too long,” said A/Prof Nadine Ezard, Clinical Director, St Vincent’s Hospital Sydney’s Drug and Alcohol Clinic.
“It’s the same whether you’re a person in the early stages of developing a drug problem or have a severe dependency issue – the services just aren’t available. We wouldn’t accept that for any other health condition.
“Between this year’s treatment service data and last year’s only an extra 3000 people managed to access publicly-funded support. The system just isn’t keeping up.
“We’re calling on governments – federal and state and territory – to boost treatment services by $1.2bn in total so we can better address unmet demand.
“We’re also asking them to develop a national plan to better coordinate services so people can get the right care, at the right place, at the right time.
“Historic under-investment in the alcohol and other drugs sector has been exacerbated by poor planning.
“In some areas, critical gaps in services are leading to crisis-oriented responses, and there can be poor integration with other clinical and social programs, with often no easy access point for help.
“The longer people wait for the help they need, the greater the damage, the higher the increased health costs, and the harder peoples’ problems are to treat,” said A/Prof Ezard.
Paul Andrews
Latest News
View all